by Nicole Brudos Ferrara
Colorectal cancer, the third leading cause of cancer-related deaths in the U.S., according to the National Cancer Institute.
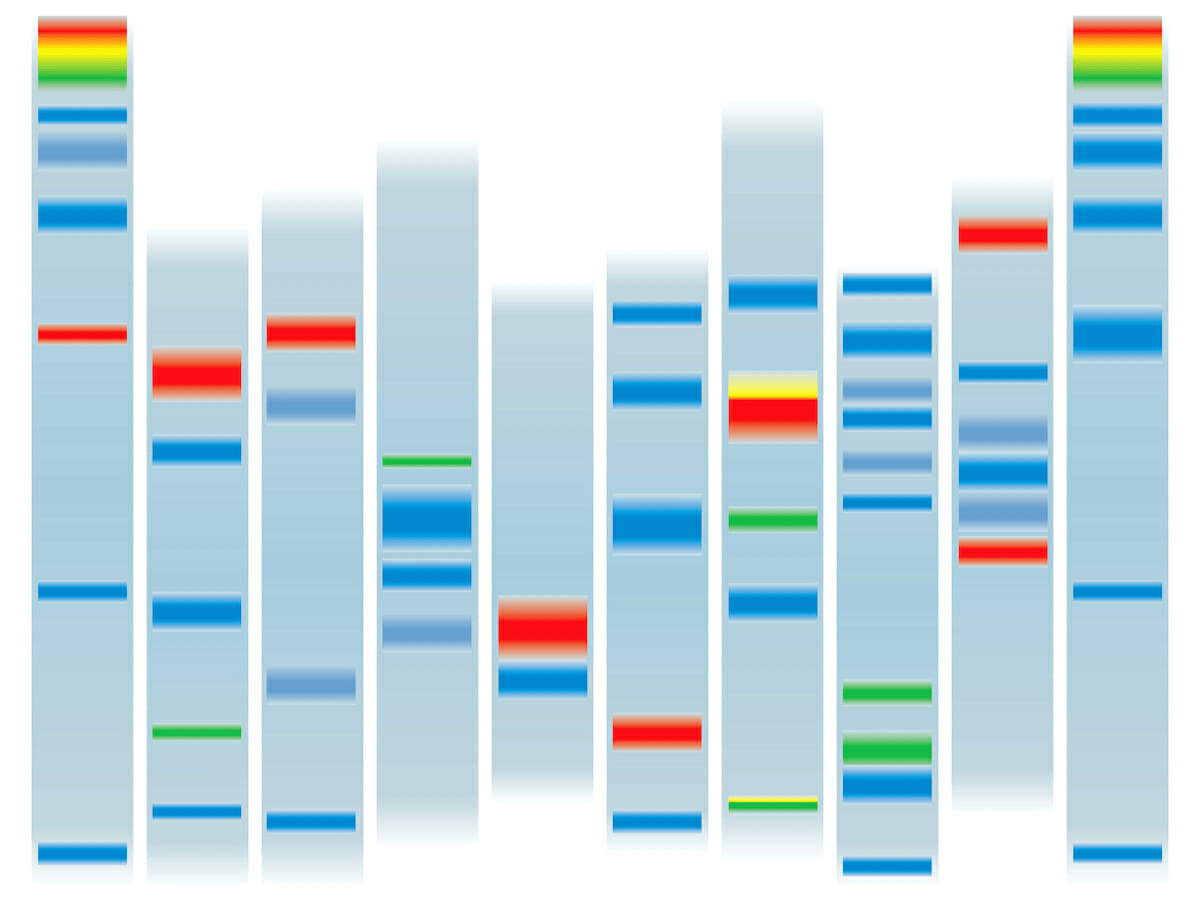
Colorectal cancer begins when healthy cells in the colon or rectum develop mutations, or changes, in their DNA. These damaged cells then become cancerous, grow and divide uncontrollably, and form a tumor. Genetic factors play a role in this process.
Some gene mutations passed through generations of your family can increase your risk of colorectal cancer significantly. The most common inherited syndromes that increase colorectal cancer risk are familial adenomatous polyposis and Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer. But you don’t need a family history of colorectal cancer to have a genetic mutation that could cause the disease.
“Someone can have developed a mutation in their germ line and be the first person in the family to have colorectal cancer,” says Lisa Boardman, M.D., a gastroenterologist and hepatologist at Mayo Clinic. “Family history is not the end of the story.”
Genetics drives development of more colorectal cancers than previously thought
Jewel Samadder, M.D., a gastroenterologist and hepatologist at Mayo Clinic, and researchers in Mayo Clinic’s Center for Individualized Medicine, recently found 1 in 6 patients with colorectal cancer had an inherited cancer-related gene mutation that likely predisposed them to the disease. In addition, the researchers discovered that 60% of these colorectal cancer cases would not have been detected using a standard guideline-based approach.
According to Dr. Samadder, these findings are important for three reasons:
- Cancer prevention. If health care professionals can identify people who have a genetic predisposition for developing colorectal cancer, they can use a colonoscopy to screen those people at an earlier age, or more frequently, to remove precancerous polyps and prevent colorectal cancer from developing.
- Family health. Health care professionals now know that most genes linked to the development of colorectal cancer are autosomal-dominant. This means that if you have a genetic predisposition for colorectal cancer, your children have a 50% chance of inheriting the genetic mutation driving that predisposition. Knowing this would help health care professionals screen those in your family at highest risk of developing colorectal cancer.
- Individualized treatment. For people diagnosed with colorectal cancer who have a genetic predisposition for the disease, health care professionals may be able to identify therapies such as immunotherapy or other drugs that can target specific molecular pathways in patients’ tumors, which can improve survival and reduce the side effects of chemotherapy.
Colorectal cancer diagnosis? Ask for genetic testing
“Anybody with a colorectal cancer diagnosis should speak to their primary care physician, oncologist or surgeon about the importance of genetic testing to identify if there was a mutated gene that predisposes them to cancer,” says Dr. Samadder. “Knowing this could potentially change the management of their cancer to improve survival—and help prevent cancer in their loved ones.”
You should know your family medical history for all cancer types, as diagnosis for one cancer could indicate that you’re at higher risk for other cancers. It’s also important to be aware of any relatives who may have been diagnosed with multiple cancers, or those who were diagnosed at a young age. Even knowing if a first-degree relative has had a polyp removed during colorectal cancer screening can be important. All these factors can play a role in your risk for colorectal and other cancers.
Knowing your family’s cancer history means you can take a proactive approach to cancer prevention.
“Anyone who has colorectal cancer should get genetic screening,” agrees Dr. Boardman. “Even if you have no family history of colorectal cancer, we still recommend it.”
Genetic testing for Lynch syndrome is particularly important. Lynch syndrome is an inherited condition that increases your risk of colon and endometrial cancers, and several other cancers. Lynch syndrome also causes cancers to occur at an earlier age than they might in the general population.
If you have Lynch syndrome, your children have a 50% chance of having it as well, as do other first-degree relatives.
If you’ve been diagnosed with colorectal cancer, these three steps are recommended:
- Talk to your health care professional about genetic testing and ask if genetic counseling is available.
- If your health care professional doesn’t offer genetic testing or genetic counseling, find a genetic counselor in your area. The National Society of Genetic Counselors website offers a directory of counselors you can search.
- Seek a second opinion at a National Cancer Institute-designated cancer center in your state. These cancer centers are funded by the National Cancer Institute to deliver cutting-edge cancer treatments to patients.
Research conducted by physician-scientists has led to improvements in prevention and treatment, and the survival of more people diagnosed with colorectal cancer. The five-year survival rate in the U.S. is now 64.7%, and death rates have been falling on average 2% each year from 2010 to 2019, according to the National Cancer Institute.
Sources: https://cancerblog. mayoclinic.org/2022/03/10/what-you-should-know-about-genetics-colorectal-cancer/
https://findageneticcounselor. nsgc.org/
https://www.cancer.gov/research/ infrastructure/cancer-centers
Exclusive content from CARE magazine