Registered nurse Latoya Bryan only has to step on a scale to measure the success of a community wellness initiative started at her church a year ago by Beaufort Memorial Hospital.
The Yemassee resident — one of the volunteers at the Family Worship Center trained by BMH to monitor the health of church members with chronic illnesses — has lost 30 pounds herself.

“I didn’t want to be a hypocrite,” said Bryan. “If I was going to tell people they should exercise and eat a healthier diet, I had to do it myself.”
She had another incentive as well.
“My father has diabetes and hypertension,” Bryan said. “I needed to make changes in my lifestyle and lose weight, or I was going to end up with the same health issues.”
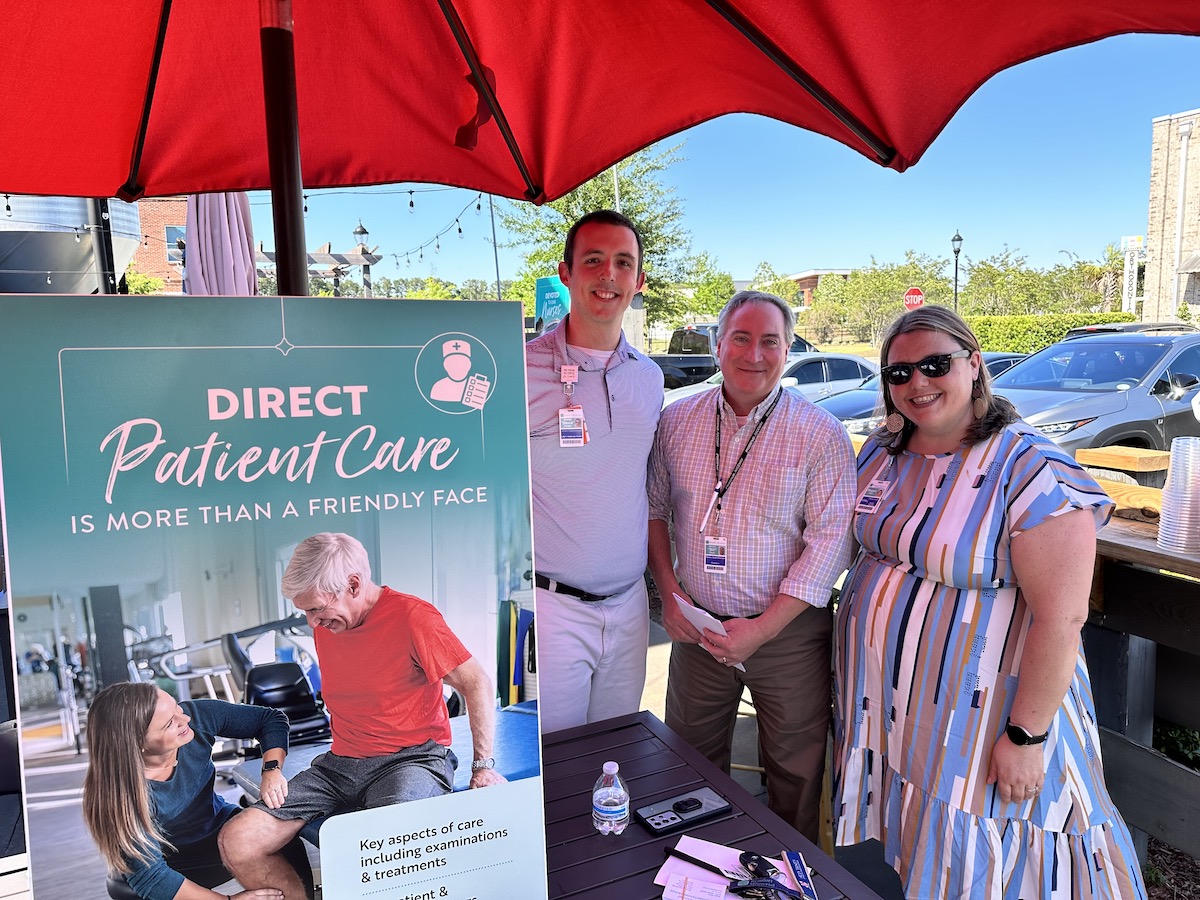
It’s been a year since Beaufort Memorial started the Transitional Care Program, funded by a grant from Duke University, to try to reduce the number of patients readmitted to the hospital for chronic diseases, specifically congestive heart failure, chronic obstructive pulmonary disease (COPD) and pneumonia.
As part of the program, a team of health care professionals, which might include a respiratory therapist, physical therapist, dietician, and pharmacist, as needed, led by a nurse practitioner, meet with patients before they leave the hospital to discuss lifestyle changes, answer questions regarding medications and educate about the disease process in general.
Additionally, the hospital makes an effort to arrange for these chronic disease patients to see a primary care practitioner after they leave the hospital so their care will continue. The next phase of the program, scheduled to be implemented later this month, will include the nurse practitioner following up with heart failure patients in their homes for 90 days post-discharge to assist in managing their care.
To reinforce the importance of compliance, BMH enlisted the help of seven area churches, many of which already had educational health programs.
“We know in the Lowcountry there is a high incidence of obesity, diabetes and high blood pressure,” said Patricia Goings, director of the Health and Wellness Ministry at Family Worship Center. “A lot of the medical problems people have are related to the southern culture.”
While lifestyle, including things like diet and cooking, is often based in tradition, Goings hopes by increasing awareness through education, residents will learn more healthy options.
Family Worship Center Health & Wellness Ministry celebrated the first anniversary of the partnership with the hospital this past weekend.
“I have to acknowledge Pastor Jeanette Harley for encouraging this ministry to exist, and her desire to empower and have all churches in the area form a Health & Wellness ministry,” said Goings.
More than 100 members of the African-American congregation have now registered for the twice-a-month screenings offered during the regular Sunday services. The volunteers conducting the tests keep a record of the patients’ blood pressure, weight, blood sugar and other vital signs, allowing them to track any deterioration in health.
“The idea is to catch a problem early before it requires hospitalization,” said Kathy Phillips, a registered nurse and diabetes educator at Beaufort Memorial’s LifeFit Wellness Center. “For instance, if a patient with congestive heart failure gains three to five pounds in a 24 hour period, it can indicate excess fluid weight gain.”
Along with training for the volunteers, BMH provided each church with medical equipment, including a stethoscope, scale and blood pressure cuff as well as a sign to promote the free screenings to the community.
Most of the volunteers using the equipment have prior medical experience. More importantly, they know the congregants participating in the program.
“Patients are more receptive to people they see every week at church than a doctor they see every three months,” Bryan said. “About 95 percent of them have made some kind of lifestyle change to improve their health.”
The screenings are free and open to the public. Participating churches include St. Helena and Faith Memorial Baptist Church on St. Helena Island, Mt. Carmel Baptist in Seabrook, Grace Chapel AME and Tabernacle Baptist in downtown Beaufort and The Link Church in Port Royal.
“It’s been a blessing. We’re helping people manage their medical issues and prevent other illnesses,” said Goings.
“Knowing that we are helping to make the difference makes it worth our time and effort to keep the program going.”