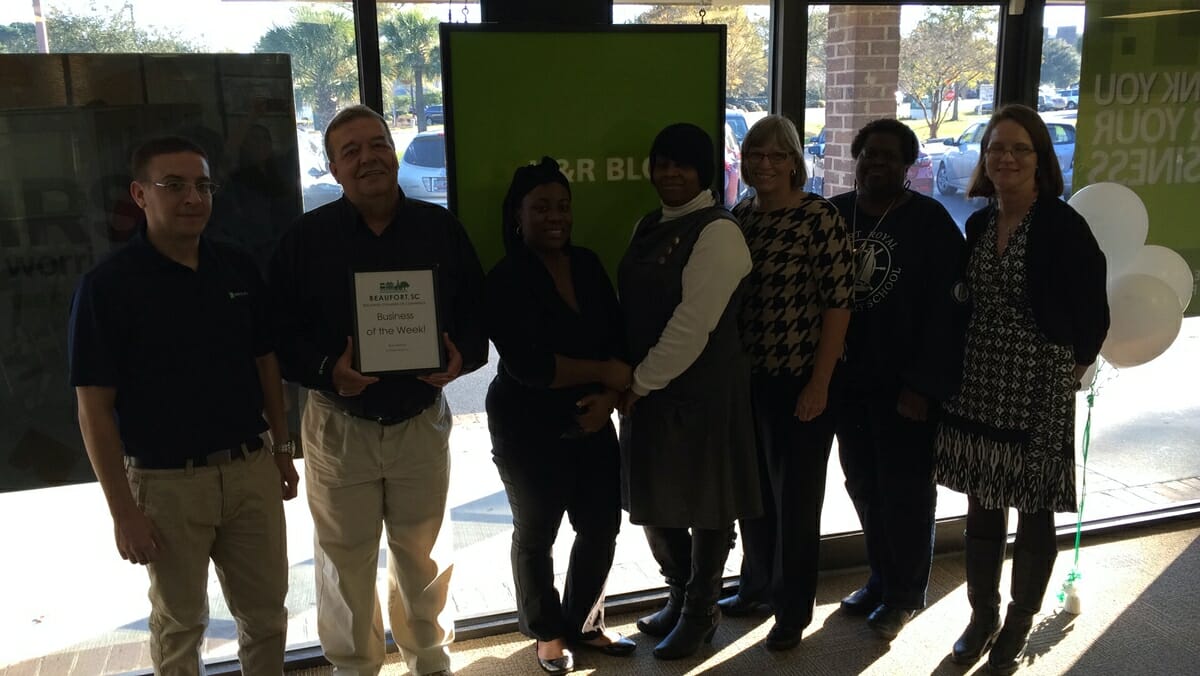
Photo above: Advanced practice providers like Paul Schaefer, PA-C and Ronda O’Connell, ANP-BC, are playing an increasingly crucial role in today’s primary care environment. “It’s a collaborative effort,” says Schaefer, a physician assistant who divides his time between Beaufort Memorial’s Lady’s Island Internal Medicine and Beaufort Primary Care. Photo by Paul Nurnberg.
Nurse practitioners and physician assistants filling a key role in today’s healthcare
Got a nagging sore throat and need medical care? Make an appointment with a nurse practitioner or physician assistant. All across the country, MDs are relying more and more on these Advanced Practice Providers (APPs) to help them meet the growing demand for primary care services.
“They’re worth their weight in gold,” said Dr. Kurt Gambla, Beaufort Memorial Hospital’s Chief Medical Officer. “They’re able to take care of routine health issues as well as a doctor and they often have more time to spend with patients.”

In the last several years, BMH has hired a dozen APPs for its busy primary care practices to better serve patients by addressing many of these routine medical needs. Several more are working with specialists in fields that include gastroenterology, vascular and general surgery, orthopaedics and obstetrics and gynecology.
“It’s a collaborative effort,” said Paul Schaefer, a physician assistant who joined Beaufort Memorial in March and currently divides his time between two of the hospital’s primary care practices. “And one of the other advantages of seeing an NP or PA is that you can usually get in faster to see them.”
The crisis in primary care developed as a result of a perfect storm of healthcare quandaries: an aging and growing population, the expansion of insurance coverage under the Affordable Care Act and fewer medical students choosing primary care as their field of medicine.
Fifty years ago, about 70 percent of all U.S. physicians practiced primary care. Today, it’s down to 30 percent. And it’s only going to get worse. At current graduation and training rates, the U.S. could face a shortage of as many as 150,000 doctors in the next 15 years, according to the Association of American Medical Colleges.
APPs are starting to fill that void. “With us in the office, there’s always someone who can see patients if the doctor is in surgery,” said Jaime Cuff, a nurse practitioner who works with BMH orthopaedic surgeon Dr. Edward Blocker. “Or we can take their hospital rounds and leave them to see patients in the office.”
While NPs and PAs take different educational tracks to get their advanced training, both can perform a wide range of preventative, acute health care services and take care of many other issues a patient might have.
They can diagnose and treat common health problems, order and interpret imaging tests and lab work, prescribe medication, refer patients to specialists and manage chronic health issues such as diabetes, high blood pressure and asthma.
“For most routine complaints, they do just as well as a physician,” said Gambla, who worked with APPs as a primary care doctor. “Having them in a practice treating minor issues leaves the physicians time to take care of more complex cases.”
Although they are always under the supervision of a doctor, some nurse practitioners and physician assistants have gone on to develop their own loyal patients.
However, many APPs like Ronda O’Connell, a nurse practitioner at Beaufort Memorial Primary Care, are still finding it necessary to educate the public on their qualifications and the role they play in today’s healthcare environment.
“But once they’ve been treated by an advanced practice provider and begin to comprehend all that we can do, they understand we have the education and training needed to take care of their needs,” she said.