SC’s mental health agency looking to increase offerings to fill gaps left by an shortage of mental health professionals
By Skylar Laird
COLUMBIA — The number of psychiatrists in South Carolina’s rural counties has plummeted over the past decade, exacerbating a lack of access to mental health services.
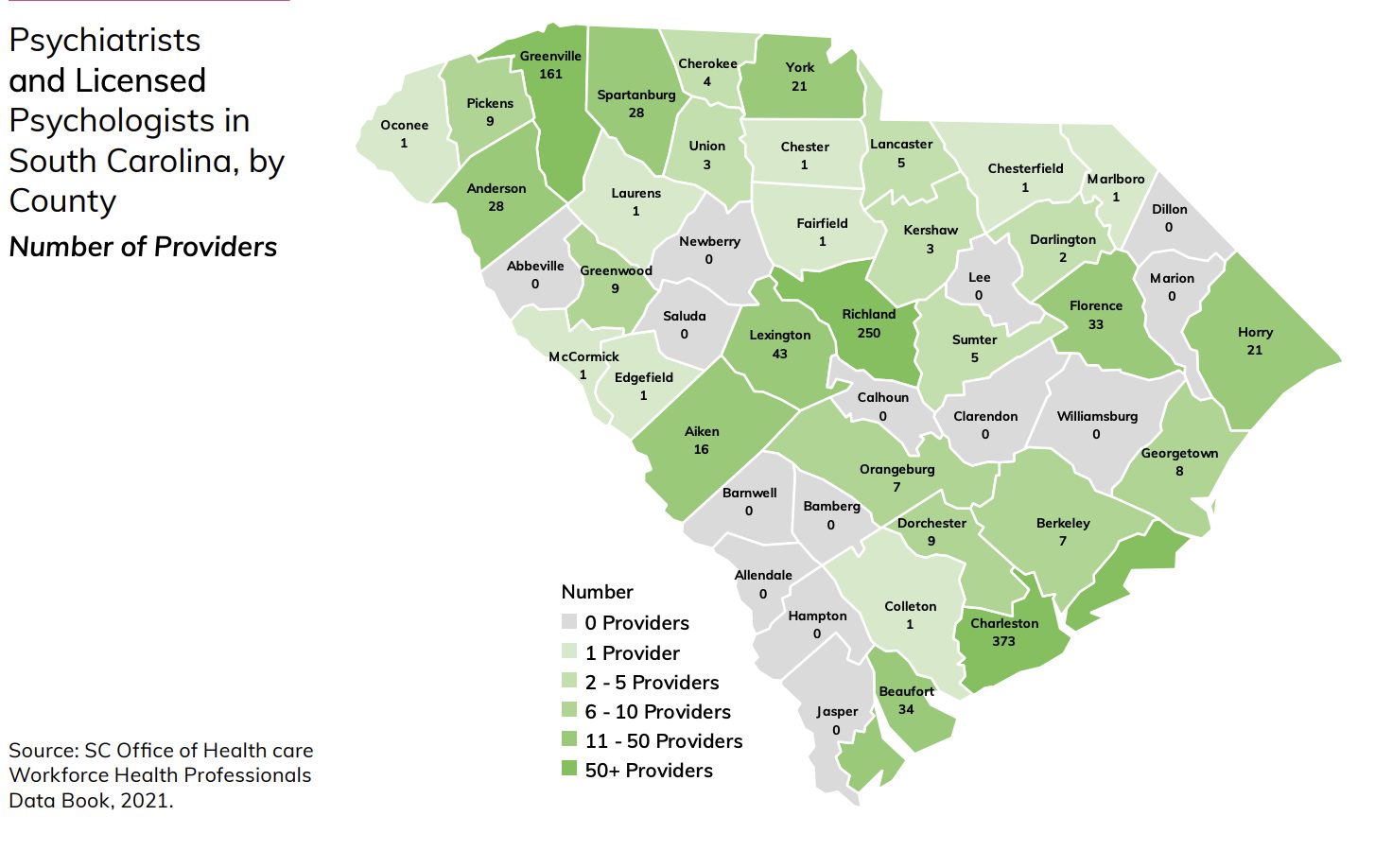
Between 2009 and 2019, the number of psychiatrists in rural areas declined by one third, the state’s annual report on health issues found, using the most recent data available. Of the state’s 46 counties, 14 had no licensed psychiatrist or psychologist in private practice, and another nine had only one. In some areas, residents have to cross multiple counties to reach a psychiatrist’s office, according to the report released last week.
State programs have been working to fill in the gaps. With public clinics, both stationary and mobile, across the state, the Department of Mental Health is seeking $3.6 million next year for programs that increase access to mental health care, officials said.
Around 20% of adults in the country have been diagnosed with a mental illness, according to the national Centers for Disease Control and Prevention. While no data definitively shows how many people in South Carolina have a mental illness, the suicide rate increased 18% between 2009 and 2018, according to the state health department’s most recently available data.
While psychiatrists and psychologists, as well as therapists and counselors, are similar, only psychiatrists can prescribe medication.
Some people are able to cope with mental health issues without medication. But for others, medication, therapy or both can be lifesaving, said Brian Wingard, spokesperson for nonprofit S.C. Thrive, which focuses on promoting healthy living by connecting people with resources.
“Breathing exercises only get you so far,” Wingard said.
Psychiatrist shortage
The drop in psychiatrists in the state’s rural areas is significant, but the number was not large in the first place, said Katie Gaul, director of the S.C. Office for Healthcare Workforce, which compiled the data. In 2009, the state had 24 psychiatrists in its rural counties; in 2019, the latest data available, that number was down to 16.
While the number of psychiatrists dropped in rural counties, the number in urban counties — Richland, Greenville and Charleston — went up 28%. As a whole, the state had 25% more psychiatrists in 2019 than it did in 2009. That increase just didn’t translate to rural areas.
Even so, the Palmetto State has a shortage of psychiatrists, Gaul said.
That leaves people, particularly those in rural areas, with few options for routine mental health care. Nearly 350,000 people, or about 7% of the state’s population, have no access to a private psychiatrist or psychologist without leaving their home county.
Those people can travel to another, more urban county, but that’s not always feasible. Some people don’t have access to transportation. Others might work full-time, preventing them from getting to offices that are often open only on weekdays. And some can’t afford the trip, especially not regularly, Wingard said.
“It’s just a massive challenge for folks to get the access to the mental health first aid they need in these areas,” Wingard said. “They’re sort of on an island.”
The shortage goes beyond South Carolina. In 2018, nearly half of all counties in the country lacked a psychiatrist, a University of Michigan study found. The problem does not have a quick fix, considering how long it takes to train a psychiatrist, Gaul said.
Psychiatrists typically spend about 12 years in school before entering the field, possibly more if they want to pursue a specialty area, Gaul said. That includes getting a graduate degree and completing a residency program.
“It’s not easy just to turn on the spigot and produce a lot more psychiatrists and psychologists,” Gaul said. “There’s a lot of lead-up time.”
Telehealth
Telehealth has been a big help for people in rural areas, said Deborah Blalock, deputy director of the mental health department’s community services.
After the COVID-19 pandemic forced many offices to shutter, health professionals in all specialties started shifting to online appointments. That means people based in places like Charleston, for example, can treat people across the state.
“I think telehealth is really the great equalizer in terms of where people live,” Blalock said.
But telehealth isn’t a fix-all. Areas without psychiatrists are often the same ones with little to no high-speed internet, making it hard, if not impossible, to access online appointments.
Recent investments in the state’s broadband network have helped. The state has invested hundreds of millions of dollars, most from federal aid packages, into expanding internet access, much of it with the express purpose of promoting telehealth.
Still, more than 190,000 homes still lacked access to high-speed internet as of March. Projects funded since are projected to bring that down to less than 134,000 by the end of December, according to the state Broadband Office.
Plus, psychiatrists may have to monitor changes in a person’s body when they start a new medication or change doses, which often requires hands-on work, like bloodwork and monitoring blood pressure, Gaul said.
“It also doesn’t help for people that really want to do an in-person visit but are limited to telehealth because there’s nobody around that they can go see, or it takes months and months to be able to get in to see someone,” Gaul said.
Filling the gaps
As the number of private mental health care professionals has dropped in rural areas, the state’s mental health department has stepped in to try and fill the gaps.
The department has 16 mental health centers, which operate 60 clinics statewide. The two counties without clinics — Saluda and Allendale — have clinics on the borders of nearby counties, so they’re still accessible, Blalock said.
“We can provide everything that we provide in the big areas in the small areas as well,” Blalock said.
On top of that, the department has 16 RVs — one for each center — that park in different places every day, in an effort to bring services into the community. And it seems to be working, Blalock said: Of the 500 or so people who got help from an RV between February 2021 and September 2022, nearly 60% had never used the department’s services before.
“It always surprises me because I’m like, ‘Well, we have clinics in all of these counties,’ yet people still aren’t making their way to the clinics,” Blalock said.
The department’s mobile crisis program, in which psychologists respond to mental health emergencies alongside law enforcement officers, also covers all of the state’s 46 counties. But the goal is to prevent crises from happening in the first place, Blalock said.
Requests for new programs
Still, there’s more the department could be doing, Blalock said. Any new programs will hinge on support in the form of funding from the Legislature.
With $1 million, state psychiatrists and psychologists would be able to do home visits for certain people diagnosed with psychotic disorders, such as schizophrenia, who need more help with everyday tasks. More than 1,700 people already qualify for the program, Blalock said.
The department runs a similar program, but the extra money would allow an expansion to see more people and do more intensive treatment for people who need it, Blalock said. The home visits are crucial to helping people before the point when they’re in crisis, she said.
Another $2.6 million would allow the department to hire 32 more mental health professionals, two per state treatment center, to work with kids and teenagers having trouble with their mental health. Like the home visits, the program would be preventative, Blalock said.
Both would cover every county in the state in an effort to ensure people have access to the resources they need, Blalock said.
“I think the philosophy of (the Department of Mental Health) is, we can provide the best services in the universe, but if people can’t access them, they’re worthless,” Blalock said. “So, our big focus is on access.”
Incentives encouraging mental health professionals to practice in rural areas, similar to those the state offered primary health doctors last year, could help address some of the disparity, Wingard said. But any programs can make a difference, he said.
“There are so many different obstacles and challenges and barriers in the way, so really any way that we can make some progress on it helps,” Wingard said.
Skylar Laird covers the South Carolina Legislature and criminal justice issues. Originally from Missouri, she previously worked for The Post and Courier’s Columbia bureau.