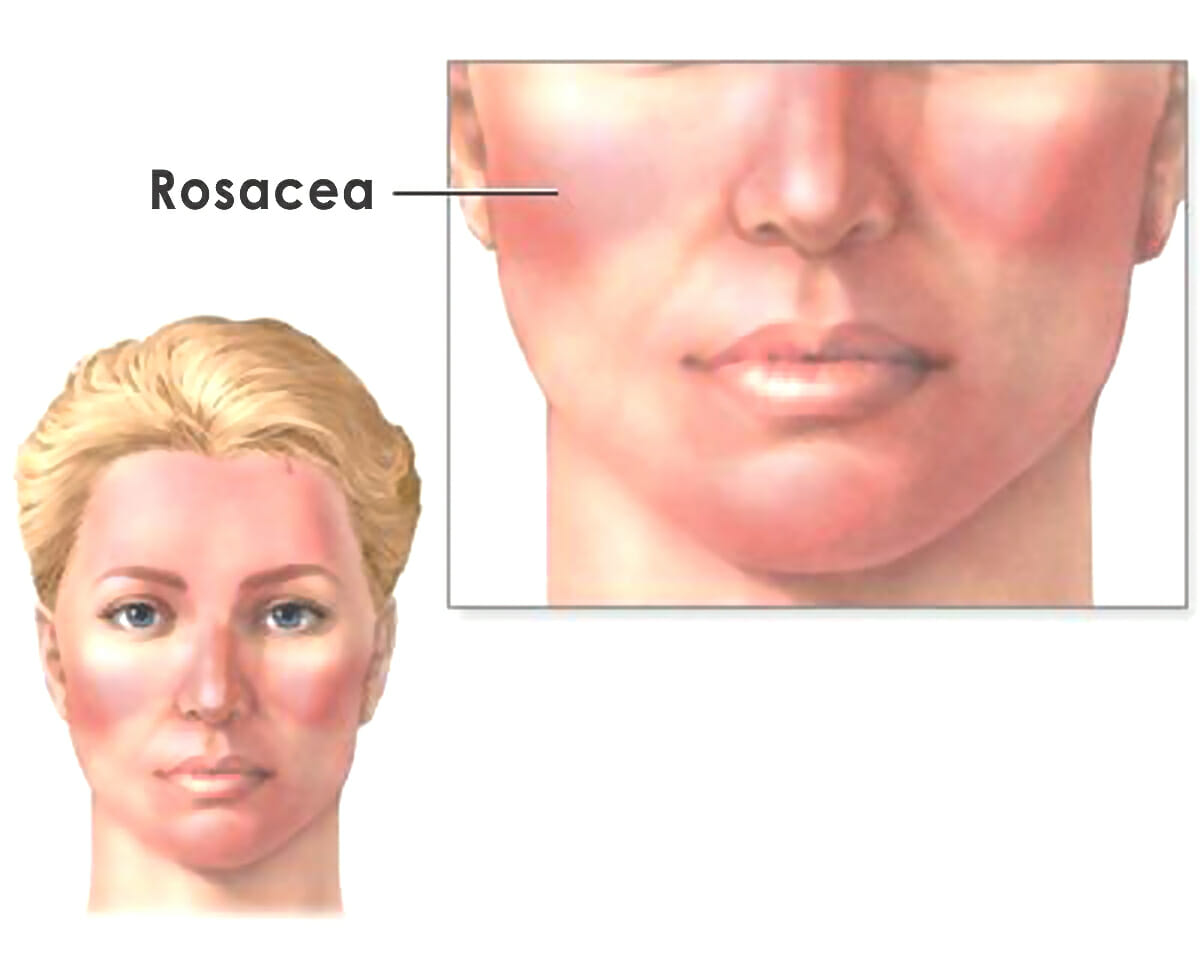
disorder of the facial skin with various potential signs and symptoms, often characterized by flare-ups and remissions. It typically begins at any time after age 30 as a flushing or redness on the cheeks, nose, chin, or forehead that may come and go. Over time, the redness tends to become ruddier and more persistent, and small blood vessels may appear. Without treatment, bumps and pimples often develop, and in severe cases the nose may become swollen from excess tissue. In around half of patients, the eyes are also affected, feeling irritated and appearing watery or bloodshot. Anyone who suspects they may have rosacea is urged to see a dermatologist for diagnosis and appropriate therapy.
The fact that certain foods can trigger a flare-up in some rosacea patients is well known. In reaction to these foods and other environmental factors such as sun exposure or extreme temperatures, the body releases substances in the skin that cause a chain reaction that leads to flushing, inflammation and, for some, burning and stinging sensations. However, although the outcome may be the same, different foods trigger different processes, according to a presentation at the American Academy of Dermatology’s recent virtual annual meeting.
“We know that sun, hot beverages, chocolate, spicy food and alcohol—many “fun” things in life—can exacerbate rosacea,” said Dr. Vivian Shi, associate professor of dermatology at the University of Arkansas for Medical Sciences. “But something that we don’t hear a lot about is that cold and formaldehyde-containing foods may also affect rosacea.”
Formaldehyde occurs naturally in small amounts in many fruits and vegetables, such as papayas, oranges, pears and bananas, as well as in fish, meat and poultry, milk, sugar and coffee. The chemical is widely used as preservative to kill micro-organisms such as bacteria, to extend shelf-life and as a defoaming agent for food processing. While it can be toxic in large quantities, the amount present in food is typically well within safe levels. People’s response to consuming formaldehyde-containing foods varies; therefore, some experience rosacea while others do not.
Through National Rosacea Society (NRS) grant-funded research, it’s now known that triggers such as spicy foods and alcohol cause keratinocytes, the most common cell type in our outermost layer of skin, and causes mast cells to release histamines and cathelicidins, both part of the innate immune system responsible for the body’s ability to combat illness. These natural substances act by eliminating harmful bacteria and activating other parts of a complex immune reaction, but inflammation is the unfortunate side effect. Researchers have discovered that cathelicidins may cause inflammatory bumps and pimples as well as vascular effects such as flushing. Studies have found that cathelicidins are more abundant in the skin of people with rosacea compared to those without the disease.
In contrast, cold beverages and formaldehyde-containing foods—as well as mustard oil and cinnamaldehyde, the organic compound that gives cinnamon its flavor—trigger the release of a different protein, which interacts with sensory neurons.2 Similarly to TRPV4, TRPA1 causes an increase in substance P and mast cell production of histamine and cathelicidin, leading to flushing and inflammation, as well as itching sensations.3
A third inflammatory reaction is triggered by foods that contain niacin, such as poultry, tuna, peanuts and crustaceans. These foods cause Langerhans cells, which are part of the immune system in the skin, to release prostaglandins, hormone-like compounds that can cause redness, inflammation and pain.
While foods containing these substances may cause flare-ups for some people with rosacea, each individual’s case is unique, and it’s usually not necessary to avoid every potential trigger. Instead, rosacea patients are advised to pay attention to their diet, make note of foods or ingredients that seem to cause a reaction in their individual cases and avoid them going forward.
The NRS offers a “Rosacea Diary” to help patients track foods as well as weather, activities and other factors that may affect their condition. Rosacea sufferers may download the diary free of charge from the NRS website at rosacea. org, or order a physical copy by writing the National Rosacea Society, 111 Lions Dr., Suite 216, Barrington, Illinois 60010; via email at info@ rosacea.org; or by calling its toll-free number at 1-888-NO-BLUSH.
The National Rosacea Society is the world’s largest organization dedicated to improving the lives of the estimated 16 million Americans who suffer from this widespread but poorly understood disorder. Its mission is to raise awareness of rosacea, provide public health information on the disorder and support medical research that may lead to improvements in its management, prevention and potential cure. More information may be found online at rosacea.org.
References:
1. Mascarenhas NL, Wang Z, Chang YL, Di Nardo A. TRPV4 mediates mast cell activation in cathelicidin-induced rosacea inflammation. J Invest Dermatol 2017;137:972-975.
2. Aubdool AA, Brain SD. Neurovascular aspects of skin neurogenic inflammation. J Investig Dermatol Symp Proc 2011 Dec;15(1):33-39. doi: 10.1038/jidsymp.2011.8.
3. Choi JE, Di Nardo A. Skin neurogenic inflammation. Semin Immunopathol 2018 May;40(3):249–259. doi: 10.1007/s00281-018-0675-z.
4. Yuan X, Huang X, Wang B, et al. Relationship between rosacea and dietary factors: a multicenter retrospective case-control survey. J Dermatol 2019 Mar;46(3):219-225. doi: 10.1111/1346-8138.14771. Epub 2019 Jan 18.
Exclusive content from CARE Magazine