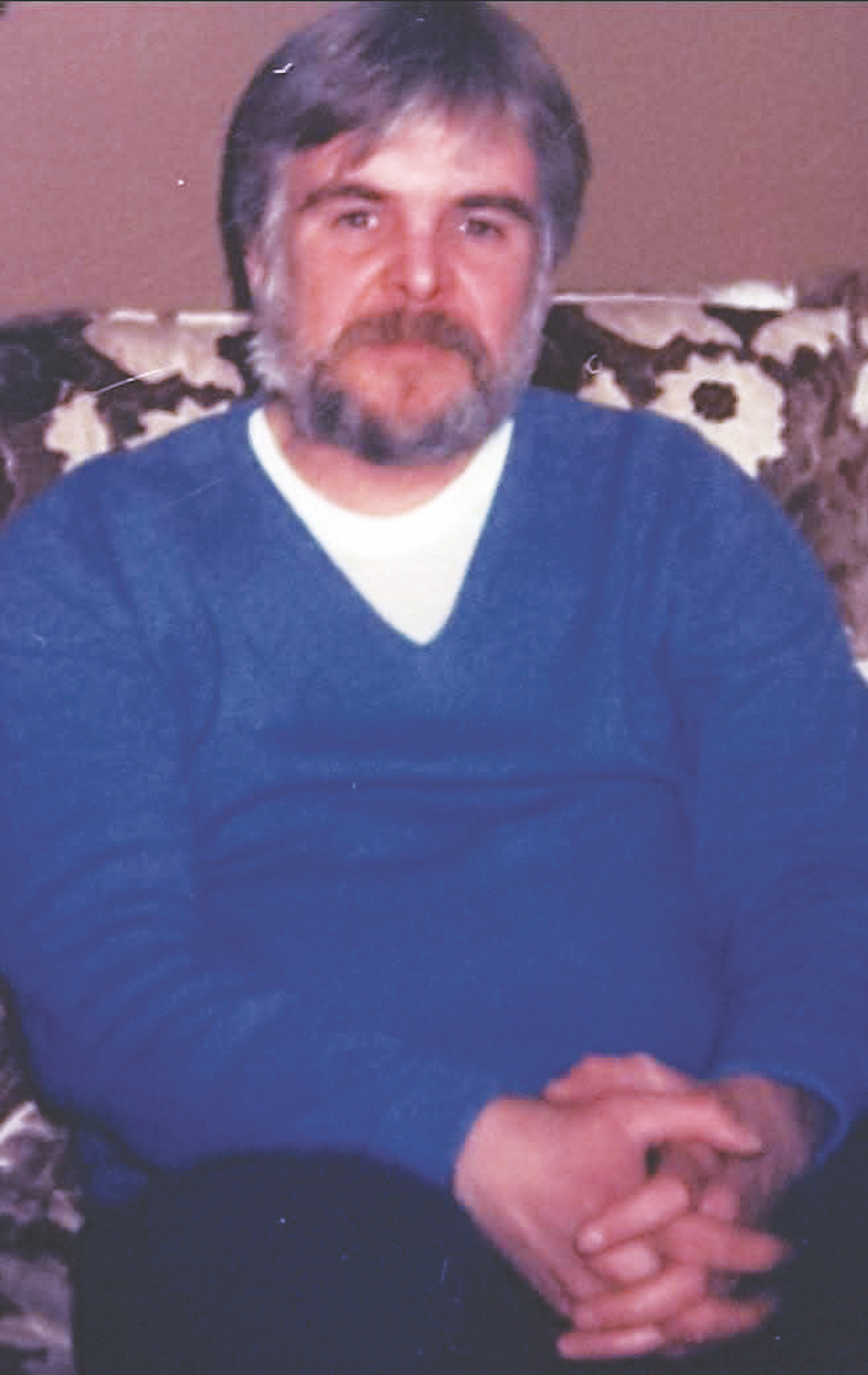
Charles Wood never saw it coming. By all accounts, the Naval Hospital Beaufort maintenance supervisor was a healthy 59-year-old man.
“I took no medications whatsoever,” Wood said. “Except for the occasional cold, I was never sick.”
So, when his right hand went numb one afternoon while he was working on his computer, he assumed it had just fallen asleep. Within minutes, the numbness had crept up to his elbow and then to his shoulder.
“It was like my arm wasn’t there,” he said. “I thought, oh shoot, I’m in trouble.”
Before he knew what hit him, his eyesight became blurry and his right leg went out on him, causing him to fall to the floor. Hearing him yell for help, his wife Chris came into the room and immediately realized what was happening. She asked him to smile to see if his face was drooping—one of the signs of a stroke.
“I couldn’t smile or stick out my tongue,” Wood recalled. “I was scared. I knew I was having a stroke.”
Not 15 minutes after Wood arrived in Beaufort Memorial Hospital’s Emergency Department, he was being virtually examined by a stroke expert from Charleston thanks to MUSC Health’s Telestroke program.
The physician was able to ask Wood questions and see his symptoms via an oversized computer screen. After reviewing his brain imaging studies, the neurologist confirmed Wood was having an ischemic stroke. About 87 percent of all strokes are ischemic, caused when a blood vessel to the brain is blocked by a clot.
According to current guidelines published by the American Heart Association and the American Stroke Association, clot-busting medication should be started within 180 minutes of symptom onset with a goal of 60 minutes from the patient’s arrival in the hospital. Wood received the life-saving drugs in 48 minutes.

“Two million neurons are lost every minute blood flow is blocked to the brain,” said MUSC Health Telestroke program manager Ellen Debenham. “It can lead to some devastating disabilities.”
Beaufort Memorial is one of 18 hospitals across the state participating in the MUSC Health Telestroke program, part of a statewide initiative focused on reducing the incidence of stroke and augmenting provision of acute stroke care in South Carolina.
“The stroke program is one of the first services to offer telehealth,” Debenham said. “It’s really the wave of the future.”
The potentially life-saving network connects partnering hospitals with immediate, round-the-clock access to MUSC Health’s stroke care experts. With the activation of this network, almost all of South Carolina is within an hour of expert stroke care. To date, the MUSC Health Telestroke program has provided expert consultative care to some 6,000 stroke patients in South Carolina.
“We’re averaging 15 patients a month that can now receive an urgent consultation,” said Beaufort Memorial Hospital stroke coordinator Sheri O’Brien.
BMH Emergency Department physicians are consulting with MUSC experts even in cases where they suspect a patient is having a “mini-stroke” known as a transient ischemic attack (TIA). While TIAs generally do not cause permanent brain damage, they are a serious warning sign that a stroke may happen in the future.
“If we know a patient has had a TIA, we can get them on blood-thinning medication and recommend lifestyle changes that could prevent another stroke,” O’Brien said.
The fifth leading cause of death in the United States, stroke ranks as the No. 3 killer in South Carolina, part of an 11-state region in the United States known as the Stroke Belt.
“We have three great neurologists in Beaufort, but it’s difficult for them to be available immediately in our Emergency Department 24/7,” O’Brien said. “With the telemedicine cart, we can reach an MUSC Health neurologist within 10 minutes.”
Less than 48 hours after being wheeled into the BMH Emergency Department on May 3rd, Wood was discharged from the hospital with virtually no deficits. He was back to work in a week.
Since his initial treatment in the hospital, Wood has continued to receive follow-up care from a Beaufort Memorial neurologist. After seeing a physical therapist, he was able to regain full dexterity in his right hand, allowing him to once again enjoy his favorite hobby—playing the guitar and piano.
“I feel fantastic,” the Port Royal resident said. “I’m very grateful for what the ER staff did for me that day. They worked like ants. Their fast response saved me from having any permanent damage.”