Wild animals usually avoid people. They might attack, however, if they feel threatened, are sick, or are protecting their young or territory. Attacks by pets are more common. Animal bites rarely are life-threatening, but if they become infected, you can develop serious medical problems.
To prevent animal bite wild animals usually avoid people. They might attack, however, if they feel threatened, are sick, or are protecting their young or territory. Attacks by pets are more common. Animal bites rarely are life-threatening, but if they become infected, you can develop serious medical problems.
To prevent animal bites and complications from bites:
- Never pet, handle, or feed unknown animals
- Leave snakes alone
- Watch your children closely around animals
- Vaccinate your cats, ferrets, and dogs against rabies
- Spay or neuter your dog to make it less aggressive
- Get a tetanus booster if you have not had one recently
- Wear boots and long pants when you are in areas with venomous snakes
If an animal bites you, clean the wound with soap and water as soon as possible. Get medical attention if necessary.
Source: Centers for Disease Control and Prevention; https://medlineplus.gov/animalbites.html
Animal bites, First aid (By Mayo Clinic Staff)
To care for a minor animal bite or claw wound, such as one that only breaks the skin, take these steps:
- Wash the wound thoroughly with soap and water.
- Apply an antibiotic cream or ointment and cover the bite with a clean bandage.
- The wound is a deep puncture or you’re not sure how serious it is.
- The skin is badly torn, crushed or bleeding significantly—first apply pressure with a bandage or clean cloth to stop the bleeding.
- You notice increasing swelling, redness, pain or oozing, which are warning signs of infection.
- You have questions about your risk of rabies or about rabies prevention. If the bite was caused by a cat or a dog, try to confirm that the animal’s rabies vaccination is up to date. If the bite was caused by a wild animal, seek advice from your doctor about which animals are most likely to carry rabies.
Bats often carry rabies and can infect humans without leaving obvious signs of a bite. This is why the Centers for Disease Control and Prevention recommends that people in contact with bats—or even those who are sleeping and awaken to find a bat in the bedroom—seek medical advice about rabies shots, even if they don’t think they’ve been bitten.
- You haven’t had a tetanus shot in the past 10 years—or five years if the wound is deep or dirty. You may need a booster shot.
SOURCES: Bats. Centers for Disease Control and Prevention. https://www.cdc.gov/rabies/exposure/animals/bats.html. Accessed Sept. 29, 2020.
Baddour LM, et al. Animal bites (dogs, cats, and other animals): Evaluation and management. https://www.uptodate.com/contents/search. Accessed Sept. 29, 2020.

Jellyfish Stings, First Aid
Jellyfish swim in waters off beaches and so pose a risk to human swimmers. When their tentacles touch skin, they pierce the skin and release a pain-causing substance. Treatment involves removing the tentacles and stopping the pain; both can be hard to do! Allergic reactions are possible, too.
Although most jellyfish are not especially dangerous to people, some are extremely toxic. Portuguese man-of-war is not actually a jellyfish but rather a colony of small, predatory animals (hydrozoan). However, due to their similarity with jellyfish, this information applies to Portuguese man-of-war stings as well.
Signs and Symptoms
A jellyfish itself consists of a bell shape with suspended tentacles. They open and close their bell-like body to drift and slowly swim in the water. The sting of a jellyfish may appear swollen, red, and bleeding. The affected area may burn and feel painful.
First Aid Guide
The rescuer should take care to avoid injury by wearing gloves and protective clothing or any readily available barrier.
- Remove the affected individual from the water.
- Wipe stingers or tentacles off with a towel.
- Wash the affected area with salt water.
Some self-care measures will help some jellyfish stings but will cause an adverse reaction in other types. For that reason, the following should be avoided without advice from a medial professional.
- DO NOT wash or soak the affected area with fresh water if the injury occurred in salt water.
- DO NOT apply vinegar, urine, alcohol, or meat tenderizer/water solution to the affected area.
- DO NOT rub the affected area.
- DO NOT raise the affected area above the level of the heart.
- DO NOT give the person medication.
Seek medical care if the person is having difficulty breathing, is bleeding profusely, or other body-wide (generalized) symptoms are occurring, such as the following: Nausea or vomiting; Paralysis; Sweating; Weakness; Cramps; Diarrhea. Also seek medical care if there is pain in an area not directly affected by the jellyfish sting, such as the groin or armpit
Snakebites, First aid (By Mayo Clinic Staff)
Most snakes aren’t dangerous to humans. Only about 15% worldwide and 20% in the United States are venomous. In North America, these include the rattlesnake, coral snake, water moccasin and copperhead. Their bites can cause severe injuries and sometimes death.
If a venomous snake bites you, call 911 or your local emergency number immediately, especially if the bitten area changes color, begins to swell or is painful. Many emergency rooms stock antivenom drugs, which may help you.
If possible, take these steps while waiting for medical help:
- Move beyond the snake’s striking distance.
- Remain still and calm to help slow the spread of venom.
- Remove jewelry and tight clothing before you start to swell.
- Position yourself, if possible, so that the bite is at or below the level of your heart.
- Clean the wound with soap and water. Cover it with a clean, dry dressing.
- Don’t use a tourniquet or apply ice.
- Don’t cut the wound or attempt to remove the venom.
- Don’t drink caffeine or alcohol, which could speed your body’s absorption of venom.
- Don’t try to capture the snake. Try to remember its color and shape so that you can describe it, which will help in your treatment. If you have a smartphone with you and it won’t delay your getting help, take a picture of the snake from a safe distance to help with identification.
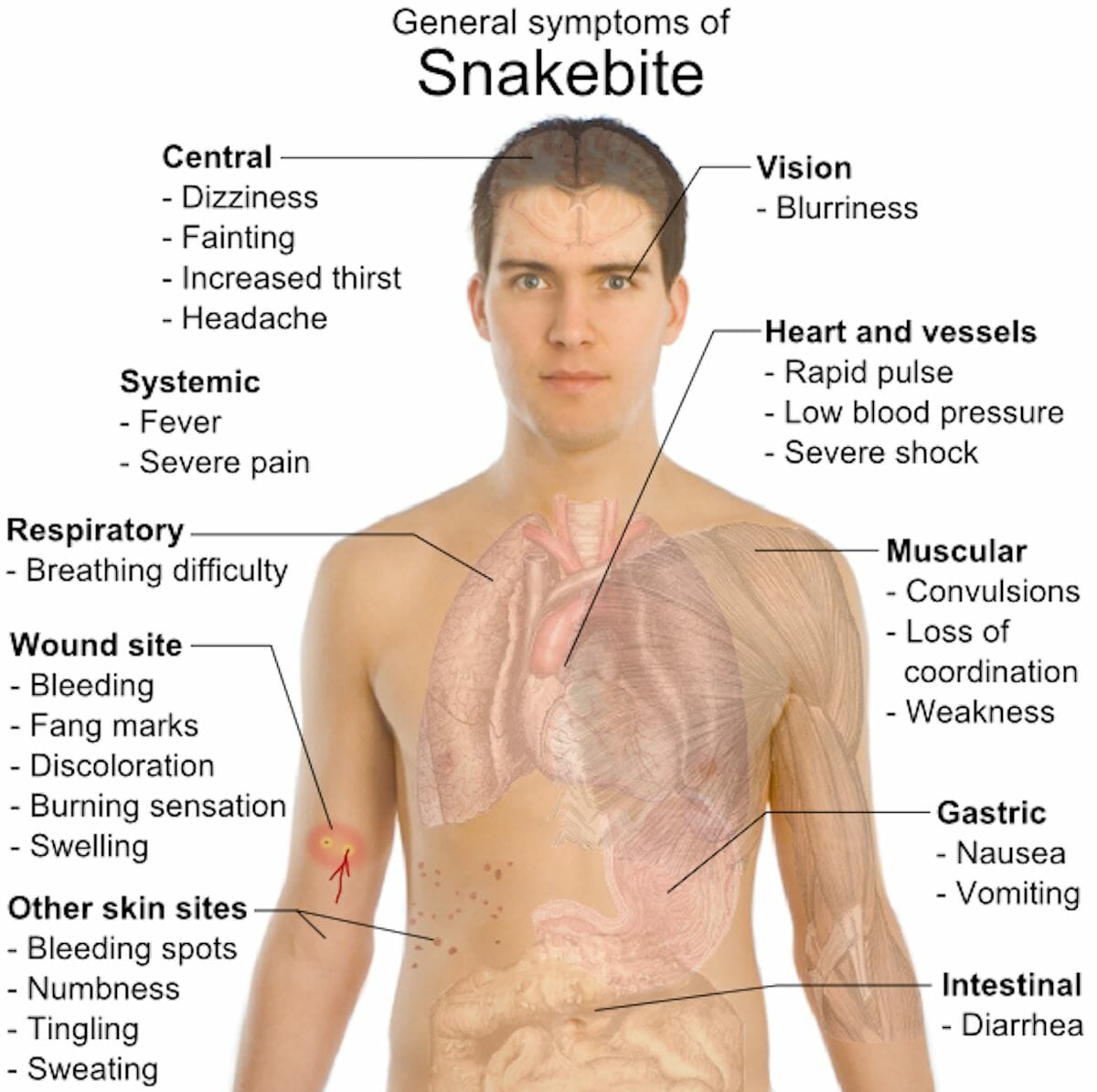
Most snakebites occur on the extremities. Typical symptoms of the bite from a nonvenomous snake are pain and scratches at the site.
Usually, after a bite from a venomous snake, there is severe burning pain at the site within 15 to 30 minutes. This can progress to swelling and bruising at the wound and all the way up the arm or leg. Other signs and symptoms include nausea, labored breathing and a general sense of weakness, as well as an odd taste in the mouth.
Some snakes, such as coral snakes, have toxins that cause neurological symptoms, such as skin tingling, difficulty speaking and weakness.
Sometimes, a venomous snake can bite without injecting venom. The result of these “dry bites” is irritation at the site.
Most venomous snakes in North America have eyes like slits and are known as pit vipers. Their heads are triangular and they have fangs. One exception is the coral snake, which has a rounded head and round pupils. Nonvenomous snakes typically have rounded heads, round pupils and no fangs.
SNAKEBITE SYMPTOMS PHOTO CREDIT: WildBackPacker.com
SOURCES: Snakebites. Merck Manual Professional Version. https://www.merckmanuals.com/professional/injuries-poisoning/bites-and-stings/snakebites?query=snake%20bite. Accessed June 24, 2019.
Papadakis MA, et al., eds. Poisoning. In: Current Medical Diagnosis & Treatment 2019. 58th ed. New York, N.Y.: McGraw-Hill Education; 2019. https://accessmedicine.mhmedical.com. Accessed June 24, 2019.
Seifert SA. Evaluation and management of Crotalinae (rattlesnake, water moccasin [cottonmouth], or copperhead) bites in the United States. https://www.uptodate.com/contents/search. Accessed June 24, 2019.
Venomous snakes. Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/topics/snakes/. Accessed June 24, 2019.
Venomous snakes: Types of venomous snakes. Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/topics/snakes/types.html. Accessed June 24, 2019.